Researchers looking for a missing cause of a common type of mutation in breast cancer cells have uncovered the biochemical culprit and found that it may also be a general source of mutation in other cancer types.
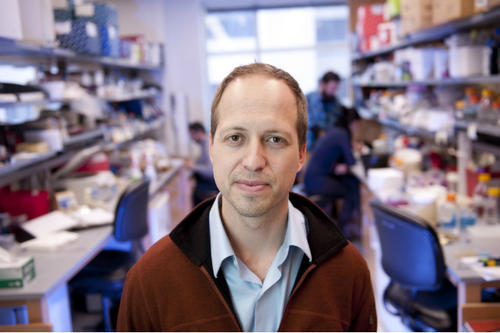
Reporting in the scientific journal Nature Communications, University of Minnesota researcher Reuben Harris and colleagues found that an enzyme known as APOBEC3H-I is the most likely cause of these previously unexplained mutations. Harris is a professor in the University’s College of Biological Sciences, a Howard Hughes Medical Institute Investigator and a member of the Masonic Cancer Center.
In breast cancer the solution became apparent in tumors lacking a related enzyme called APOBEC3B. All breast tumors with an APOBEC mutation footprint have APOBEC3B and, if they lack this enzyme due to a naturally occurring deletion, they invariably have APOBEC3H-I. The mutational contribution of APOBEC3H-I was also clear in lung cancer, in addition to expected mutational footprints from tobacco smoke and ageing.
These findings are important because they provide a molecular explanation for a major source of mutation in many different types of cancer. The results point the way to fine-tuning the treatments of these cancers by inhibiting these enzymes in order to limit the development of mutations that undermine many current cancer therapies.
“Our results encourage the development of new cancer treatments that work by combining existing therapies and an APOBEC inhibitor to stop tumor cells from evading therapy by developing resistance mutations,” Harris said.
The findings are based on the fact that cancer begins when the genetic material inside a cell mutates, causing the cell to change and indiscriminately multiply. The processes that cause these mutations — say, ultraviolet light in the case of skin cancer or smoking in the case of lung cancer — leave a characteristic signature or footprint. The second-most common mutation type (behind ageing) is that caused by the APOBEC enzymes. These enzymes are normally beneficial by helping to kill viruses, but the same DNA-mutating trait that makes them good at this job can also give them the ability to contribute mutations to tumor evolution if they become too abundant and/or misregulated.
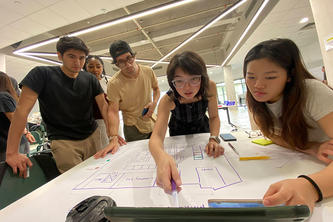
Past research led by Harris showed that APOBEC3B is a source of mutations in breast cancers with APOBEC footprint. However, Harris and others also found that some breast tumors still have an APOBEC footprint but no APOBEC3B. To find out why, Harris, the lead author Gabriel Starrett, and collaborators from the University of Minnesota Masonic Cancer Center, the Howard Hughes Medical Institute, and the University of Saskatchewan began looking at variants of another APOBEC family member known as APOBEC3H. They were surprised to find that what was thought to be a relatively unstable, inactive variant known as APOBEC3H-I is likely the culprit. This protein is found in tumor cells with APOBEC signatures, and it is also much more active than expected from prior studies. APOBEC3H-I can access the nuclear DNA of the cell, providing a molecular explanation for its role in cancer mutagenesis.
Armed with the knowledge of APOBEC3H-I’s role in cancer, Harris is now looking to learn more about how this enzyme actually induces mutations. “We would like to better understand the underlying molecular mechanism,” he said. “As with any new process, a better understanding of the molecular details will provide additional angles for future therapies.”
- Categories:
- Science and Technology