On Thanksgiving morning 1981, Marilyn and Charles Fiske of Bridgewater, Massachusetts had much to be thankful for: a newborn bundle of joy named Jamie.
Before long, however, the Fiskes were wondering if Jamie would see a second Thanksgiving. The baby had biliary atresia, a fatal blockage of the bile ducts in the liver that could only be cured by a liver transplant.

Desperate, the Fiskes reached out to the University of Minnesota and liver transplant surgeon John Najarian, who had been building the U of M transplant program toward international leadership since the late ‘60s. He agreed to help them, but a donor still had to be found.
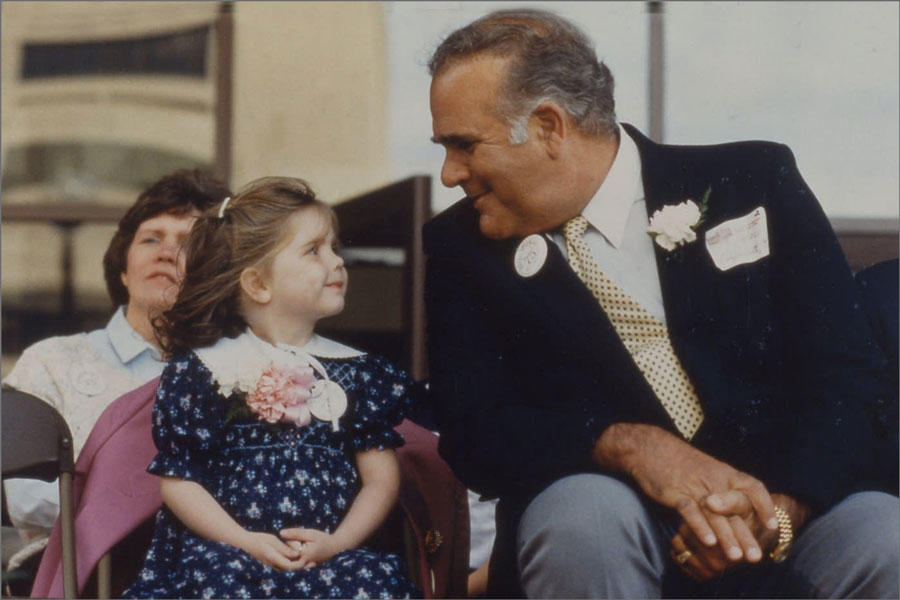
Charles Fiske secured a chance to address the pediatricians gathered at a meeting of the American Pediatrics Association in New York. Urging the doctors to keep an eye out for a donor, he said that Jamie’s favorite song was “You Are My Sunshine.”
“She is my sunshine,” he told the hushed audience.
With Jamie just a day or two from death, a donor—a baby boy who died in Utah—was found. Still, no child as young as Jamie—11 months—had ever received a successful liver transplant. It meant connecting blood vessels only a millimeter or two wide and a high likelihood of surgical complications.
On November 5, 1982, Najarian swept all that aside.
“I took a chance for Jamie,” he said.
Forty years later, Jamie Fiske stands as a living testament to the skill of Najarian and the U of M Liver Transplant Program, whose record in recipient survival ranks in the top 10 percent of such programs in the nation, according to the Scientific Registry of Transplant Recipients. But while her story made history, it also owed a great debt to foundational discoveries by University researchers. Since the 1960s, when the first successful kidney transplants in Minnesota were done at the University Hospitals, the U of M has housed one of the world’s oldest and most successful transplant programs.
As the University nears its 13,000 transplants milestone, a few highlights of its continuing journey show the depth and breadth of its leadership roles.
Setting the stage

The discoveries of Robert Good, a U of M alumnus and Medical School faculty member (1950-1972), laid the groundwork for understanding the immune system and how it distinguishes “self” from “foreign” tissue.
Good’s work revealed the dual nature of the immune system and how immune cells develop and interact, and also illuminated the key role of the thymus gland. In 1968 Good performed the first successful bone marrow transplant from a matched related donor, on a baby with a severe immune deficiency.
The U of M led the drive to prevent rejection, says Arthur Matas, a professor and kidney transplant specialist in the Department of Surgery.

The U of M led the way to making donations from living donors the norm, leading to many of the program's successes in kidney transplantation, including transplantation to help diabetic patients, infants and children. The program is unique in doing long-term follow-up of living donors, and showed in 1992 that living kidney donors fared as well in the long term as their siblings.
The program also pioneered transplants from "non-directed donors”—living donors who had no specific recipient in mind, but offered to donate to anyone on the waiting list.
“Previously it was thought that there must be something wrong with an individual making such an offer,” Matas recalls. “The acceptance of non-directed donors has increased living donation throughout the country.”
Pancreas pioneer

In 1974 David Sutherland, a surgical resident at the U of M, began the world’s first clinical transplants of the pancreatic insulin-producing groups of cells known as islets of Langerhans. In 1979, as an assistant professor of surgery, he performed the first living-donor partial pancreas transplant. The next year, he, John Najarian, and colleagues demonstrated that the full-blown diabetes that followed pancreatectomy (to cure chronic pancreatitis) could sometimes be prevented or partially ameliorated by isolating islets from the removed organ and infusing them back into the patients.
Sutherland went on to oversee thousands of pancreas transplants and islet autotransplants at the U of M, where he headed the world’s oldest and largest pancreas transplant program. More than 100 of his former mentees have begun or directed pancreas/islet transplant programs worldwide. He also founded the International Pancreas Transplant Registry. Sutherland’s work was central to the U of M becoming—and remaining—a world leader in both transplant fields.
“David is widely considered a pioneer in pancreas transplantation, but to me he is also a kind-hearted person with boundless generosity, a keen intellect and sharp wit, and the desire and willingness to help anyone in need.” says Raja Kandaswamy, professor and vice chief of the Department of Surgery’s Division of Transplantation.
Transplanting talent
It’s a sure sign of leadership when an institution seeds the landscape with a steady stream of new leaders and innovators. Two examples from the U of M show how training new talent generates dividends for patients and the field of transplantation.
Surgery at the U of M gained prominence long ago, thanks in large part to two legends: Surgery Department chair Owen Wangensteen and open-heart surgery pioneer C. Walton Lillehei.
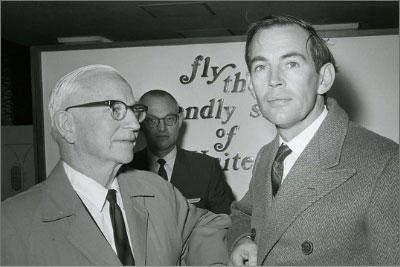

In the mid-20th century, human heart transplants were unheard of. But in 1956 Wangensteen and, especially, Lillehei took on two trainees named Norman Shumway and Christiaan Barnard. Shumway went on to pioneer, with colleague Richard Lower, techniques for human heart transplantation at Stanford University.

But in December 1967 Barnard, drawing on Shumway and Lower’s work, performed the world’s first human heart transplant. In January 1968, Shumway performed the first successful transplant in the United States.
These breakthroughs ignited intense worldwide interest in heart transplantation. However, few recipients survived beyond a few months, and surgeons soon abandoned the procedure.

But not Shumway. He and his team persisted, with innovations that included the use of cyclosporine as an anti-rejection drug. Shumway eventually oversaw some 800 heart transplants and is credited with saving heart transplantation from oblivion and ushering it into the medical mainstream.
His daughter Sara Shumway, a cardiovascular surgeon who also specializes in heart and lung transplants, is now professor and vice chief of the U of M Department of Surgery’s Division of Cardiothoracic Surgery.
She’s well aware of how her father embraced Wangensteen’s belief that surgeons should also be scientists. This fueled Norman Shumway’s drive to both research and perfect human heart transplantation.
“He and Dick Lower would do clinical work three days a week and laboratory work two days a week,” Shumway recalls. “In this way they were able to refine the surgical technique of heart transplantation and learn how to detect rejection.”
John Najarian, who succeeded Wangensteen as surgery department chair, was assisted in the Jamie Fiske operation by a physician named Nancy Ascher. The first woman to perform a liver transplant, she was recruited in 1988 by the University of California-San Francisco to start what has grown into a highly rated liver transplantation program.
“At one point I counted that people we trained were at transplant programs in 35 states and six countries,” notes Arthur Matas. “Thirteen U of M-trained transplant surgeons have been president of the American Society of Transplant Surgeons.”
A visionary’s guide to the future

Immunosuppressive drugs are well known for putting patients at greater risk for cancer, infection, and cardiovascular disease. But they also can harm the transplanted tissue. Andrew Adams, professor and chief of the Department of Surgery’s Division of Transplantation, is leading the charge to extend both the supply of available organs and the lifetimes of those organs post-transplant.
He and his colleagues have developed a drug that more specifically targets the immune system’s attacks on transplants, a step toward training the immune system to recognize transplanted tissue as “self,” not foreign.
The researchers also envision the use of imaging to catch organ rejection early on.
“When this happens, it can be very subtle and difficult to distinguish from other processes such as dehydration or infection,” Adams explains. “It typically requires an invasive biopsy procedure.”
But noninvasive imaging may, for example, detect immune cells infiltrating transplanted organs, a warning that rejection is beginning.
In a third direction, Adams is investigating the use of pig organs to supplement, or perhaps even replace, the human supply. He and his colleagues in the fledgling Porcine Transplantation Program are on to launch successful initial clinical trials of kidney, heart, and pancreatic islet cell transplantation from pigs to human patients by 2025.
Says Adams: “Our hope is that, with newer medicines and fewer side effects, a transplant can last a lifetime—and not shorten that life at all.”