Plan identifies what is necessary to ensure a rapid response to future outbreaks
The Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota released the 2024 Update of a Research and Development (R&D) Roadmap for Nipah Virus to accelerate the development of medical countermeasures (MCMs), including diagnostics, therapeutics and vaccines, to enable effective and timely emergency response to Nipah virus (NiV) outbreaks. A research paper on the roadmap, "Measures to prevent and treat Nipah virus disease: research priorities for 2024-29," by KA Moore et al., was published in the journal The Lancet Infectious Diseases.
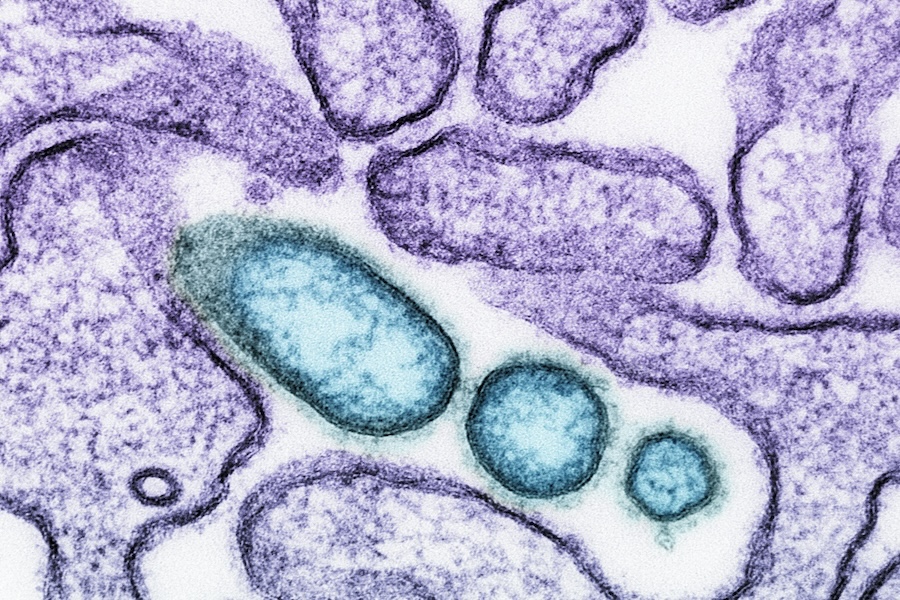
NiV was first identified after an outbreak of respiratory illness in pigs and encephalitic disease in humans occurred in Malaysia and Singapore in 1998 to 1999. NiV infection often causes severe, rapidly progressive encephalitis, which may be relapsing. The case-fatality rates range from 40 percent to 100 percent in recognized outbreaks. There currently are no treatments or licensed vaccines available to prevent or control Nipah infection.
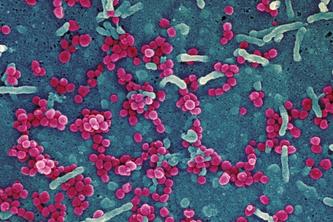
Fruit bats of the Pteropus genus are the primary natural reservoir for NiV. In the Malaysia outbreak, NiV spillover occurred from bats to pigs, which led to pig-to-pig, pig-to-human and possible limited person-to-person transmission. Additionally, researchers found that several other domestic animal species in the outbreak area were infected with NiV.
Researchers have detected similar Nipah-like viruses in other animals, suggesting that bats are not the sole reservoir and that the geographic range of such viruses may be greater than previously recognized. This wide potential range of NiV natural reservoir hosts raises concerns about the occurrence of outbreaks in new geographic areas, thereby greatly expanding the global at-risk population.
“While Nipah virus disease generally occurs only in small, focal outbreaks in South Asia, the main animal hosts for the virus are pteropid fruit bats,” said Michael Osterholm, PhD, MPH, CIDRAP director, University of Minnesota Regents Professor and McKnight Presidential Endowed Chair in Public Health. “These bats can be found across much of Asia, the Western Pacific and Africa, so much of the global population is at potential risk for this highly deadly disease.”
The 2024 update of the NiV R&D roadmap is based on scientific literature published primarily in the past five years and the consensus opinion of an expert working group with broad experience in developing MCMs for NiV or experience in epidemiology, ecology or public health control of Nipah outbreaks. It identifies current challenges and barriers that need to be addressed to ensure that NiV MSMs are developed, manufactured, and readily available, affordable, and appropriate for use in affected areas. The research priorities are organized into four main sections with key achievements that are necessary over the next six years to realize the goal of effective and available NiV MCMs by the end of this decade.
“If a strain of Nipah virus emerges that is more adaptable to humans with greater potential for person-to-person transmission, we need to have the tools in place to treat the disease and quickly contain its spread,” said Osterholm.
Examples of key milestones that cover the four topic areas in the roadmap include:
- By 2024, conduct scenario planning to identify gaps, clarify regulatory procedures and determine the acceptable pathways for approval and emergency use authorization of NiV MCMs in countries at highest risk for NiV outbreaks.
- By 2024, generate standardized and well-characterized assays, reagents, antibodies, nucleic acids, and stocks of NiV challenge strains to facilitate R&D of NiV MCMs.
- By 2024, develop and standardize plans and protocols (including the governance structure) for creating repositories of well-characterized acute and convalescent clinical samples.
- By 2024, complete an agreed-upon generic prepositioned protocol for conducting clinical trials of promising therapeutic candidates.
- By 2024, complete phase 1 clinical trials for at least three promising NiV candidate vaccines.
- By 2025, complete at least one additional phase 1 clinical trial in an NiV-affected area of a promising monoclonal antibody (mAb) or mAb cocktail to assess safety and tolerability.
- By 2025, describe the range of possible protective thresholds against NiV infection for serum neutralizing antibodies or other functional correlates of protection, which can be used in animal studies and for immunobridging to humans.
- By 2025, initiate phase 2 clinical trials, preferably in affected areas, to further assess immunogenicity and safety for at least two of the most promising NiV candidate vaccines.
- By 2027, complete clinical validation of performance and operational suitability for at least two of the most promising NiV point-of-care or near-patient diagnostic tests that align with the target product profile and can be used in peripheral sites.
- By 2028, promote international regulatory approval for at least one rapid, point-of-care or near-patient-care NiV diagnostic test that can be commercialized and standardized.
- By 2028, complete at least one phase 1 clinical trial of the preliminary safety and tolerability of at least two promising small-molecule therapeutic candidates or combination therapies for treating NiV disease.
Other overarching areas that are identified in the roadmap include the following:
- Improve global NiV surveillance capabilities in humans and animals in affected and at-risk countries.
- Complete preclinical evaluation of potential therapeutic agents and move the therapeutic pipeline toward clinical trials in affected areas.
- Develop the tools and policies necessary for evaluating and potentially approving one or more NiV candidate vaccines through a nontraditional regulatory pathway.
- Expand use of state-of-the-art techniques and tools, such as ex vivo challenge models, machine learning, artificial intelligence, computational-aided drug design, and structural biology to accelerate progress toward ensuring availability of NiV MCMs by the end of the decade.
“Our hope is that the availability of this roadmap will help galvanize global support to further advance diagnostics, therapeutics and vaccines against one of the world’s deadliest viruses,” added Osterholm.
Support for the 2024 Update of the Nipah Virus R&D Roadmap was provided by the Wellcome Trust.
About the Center for Infectious Disease Research and Policy
Part of the University of Minnesota's Research and Innovation Office, CIDRAP is a global leader in addressing public health preparedness and emerging infectious disease response. Founded in 2001, CIDRAP works to prevent illness and death from targeted infectious disease threats through research and the translation of scientific information into practical applications, policies and solutions.
- Categories:
- Health
- Infectious diseases
- Population health