In almost all cultures, seeking care for sexual health concerns can be an awkward, complex, and vulnerable experience. A key to making such care easier and more comfortable is properly training providers to compassionately and effectively deliver high-quality, medically accurate treatment, no matter where they live.
University of Minnesota researchers recently launched a collaboration to train healthcare students in socially conservative Tanzania on the best ways to treat sexual health. Tanzania has some of the highest rates of HIV, sexually transmitted infections, sexual violence, and early pregnancy in the world.
“The University of Minnesota is a world leader in providing sexual health training to health students. But it’s important to recognize that you can’t just take a curriculum that was originally designed for medical students in Minnesota and expect it to work in East Africa,” says Simon Rosser, School of Public Health professor and principal investigator. “To be maximally effective, we needed to first understand the sexual health cultural practices, challenges, and priorities in Tanzania.”
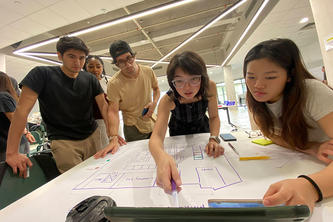
Working with a team from Tanzania, the researchers surveyed and interviewed 121 midwifery, nursing, and medical students and professionals participating in 18 focus groups. In addition, the team conducted individual interviews with local experts—including community, religious, cultural, and political leaders—to better understand the common myths and misconceptions around sexual health.
The researchers found that many conservative attitudes significantly influence how providers offer care. For example, for a case study of a woman presenting with domestic abuse injuries, some participants wondered what she had done to anger her husband and whether the beating was “justified.”
Providing health care to homosexual patients is another exceptionally sensitive issue given that homosexuality is illegal and heavily stigmatized in Tanzania. Students and providers wondered if they should report such patients to the police. Others suggested referring the patient to a psychologist to “cure” their homosexuality.
“What’s important here is to recognize how cultural and societal attitudes shape the health care practices of providers,” says Rosser. “In the absence of sexual health training, providers hold to many of the same myths and misconceptions that their patients believe. Without training, the providers cannot provide medically accurate education to patients to address the enormous sexual health challenges of patients and communities, and above all, prioritize their health.”
Rosser and his colleagues are using these and other findings to adapt the training curriculum to Tanzanian culture. Then, the researchers will test it in a randomized controlled trial of 420 healthcare students—the first such trial anywhere in the world.
- Categories:
- Health
- Human rights
- Population health